Revenue Cycle Management (RCM) is applicable to clinics and hospitals functions similarly to a financial handbook. It facilitates the tracking of patient and insurance company payments.
It begins at the moment the patient checks in. RCM ensures that all pertinent information, including insurance information and medical history, is accurately gathered from the very beginning.
It lowers errors, saves time, and simplifies tasks with the help of technology. Automated processes such as billing, payment collection, and appointment scheduling are made more accessible by RCM systems.
RCM guarantees the accuracy of billing statements. It verifies that the services rendered are accurately billed to insurance providers. This keeps hospital finances stable and helps them receive payments on time.
RCM responsibilities are sometimes outsourced. Hospitals may contract with outside companies to manage their paperwork and billing. This enables hospitals to concentrate on patient care while RCM professionals take care of the hospital finances.
Importance of RCM in Organizations
Implementing these RCM Strategies will definitely shorten the denials and increase the organization's revenue rapidly; here is the list of strategies to follow;
-
Strengthening the Patient Data Capture at First Visit.
-
Automating the workflow process.
-
Improving Billing Timeliness and Coding Processes.
-
Focus on Denied claims for faster reimbursement.
-
Outsourcing to other BPO vendors.
Strengthening the Patient Data Capture at First Visit.
When a patient steps into a hospital or clinic for the first time, several crucial actions take place to ensure accurate and comprehensive data capture. Let's break down the process step by step:
Registration and Check-In
The first point of contact is often the registration desk or reception area. Here, the patient provides basic information such as name, address, contact details, and insurance information. This initial step sets the stage for further data collection throughout the visit.
Medical History and Symptoms
After registration, the patient may be directed to a nurse or medical assistant who gathers detailed information about their medical history, current symptoms, and reason for the visit. This information helps healthcare providers understand the patient's health status and modify their care accordingly.
Vital Signs and Measurements
The next step typically involves taking essential signs such as blood pressure, heart rate, temperature, and weight. These measurements provide imperative baseline data and help identify any immediate health concerns that require attention.
Electronic Health Record (EHR) Documentation
As the patient moves through the intake process, all information collected is entered into the hospital's electronic health record (EHR) system. This digital platform serves as a centralized patient data repository that makes it possible for medical specialists to swiftly and effectively obtain pertinent information.
Insurance Verification and Authorization
In parallel with clinical assessments, staff members verify the patient's insurance coverage and obtain necessary authorizations for treatment or procedures. This step ensures that the patient's insurance information is accurate and up to date, minimizing billing errors and claim denials later on.
Consent Forms and Legal Documents
Depending on the nature of the visit, patients may be required to sign consent forms or other legal documents before proceeding with treatment. These documents outline the risks, benefits, and alternatives to proposed interventions, ensuring that patients are fully informed and involved in their healthcare decisions.
By carefully following these steps, healthcare organizations can strengthen patient data capture at the first visit, laying a solid foundation for coordinated and personalized care delivery.
Automating the Workflow Process.
In the busy world of healthcare, it's essential to keep things running smoothly. One way hospitals do this is by using software to automate tasks. Here's how:
Booking Appointments
Instead of calling to make an appointment, patients can use a website or app to book one online. They can also get reminders about their appointments, which helps them remember.
Checking In
Patients can complete the necessary paperwork online before they even arrive at the hospital, saving them time and effort when they fill it out later. When people check-in, things go more quickly and efficiently as a result.
Keeping Records
Physicians and nurses utilize computers to record patient data, such as medical histories, test findings, and treatment recommendations, rather than writing everything down on paper. Everything is conveniently located in one location in this manner.
Prescribing Medicines
Doctors can electronically email prescriptions to the pharmacy rather than writing them out by hand. Patients receive their medications more quickly, and errors are less likely to occur as a result.
Billing and Getting Paid
Hospitals utilize computer applications to send bills and insurance claims online rather than by hand. This speeds up the payment procedure for the services they provide.
Improving Billing Timeliness and Coding Processes.
Ensuring billing timeliness and accuracy is vital for the financial stability of hospitals. Here are 4 essential steps to achieve this:
Training Staff Thoroughly
Properly trained staff are essential for accurate billing and coding. Hospitals should invest in comprehensive training programs to ensure employees understand billing procedures and coding guidelines.
Regularly Audit Billing Practices
Conducting regular audits of billing practices helps hospitals identify areas for improvement and ensure compliance with billing regulations. Audits can uncover errors or inefficiencies that may be impacting billing timeliness and accuracy.
Staying Compliant with Regulations
Billing regulations can be complex and ever-changing. Hospitals must stay up-to-date with regulatory requirements to avoid penalties and claim denials. Regular compliance audits can ensure adherence to guidelines
Monitoring Accounts Receivable
Keeping track of outstanding payments is essential for financial management. Hospitals should regularly monitor accounts receivable and follow up on unpaid bills promptly to improve cash flow and revenue collection
Focus on Denied Claims for Faster Reimbursement
When hospitals send out bills to insurance companies, sometimes those claims get denied. But there are ways to speed up the process of getting paid. Here's how:
Find out Why Claims are Denied
First, hospitals need to figure out why the claims are getting denied. It could be because of coding errors, missing information, or issues with insurance coverage.
Fix Mistakes Quickly
Once hospitals know why the claims are being denied, they can fix the mistakes right away. This might involve correcting coding errors, providing additional documentation, or updating patient information.
Appeal Denied Claims
If a claim is denied unfairly, hospitals can appeal the decision. This means they ask the insurance company to review the claim again and reconsider their decision. Sometimes, claims are approved on appeal.
Keep Track of Appeals
Hospitals should keep track of all the claims they appeal. This helps them follow up with the insurance company and make sure the appeals are processed in a timely manner.
By focusing on denied claims and taking steps to resolve them quickly, hospitals can improve their chances of getting reimbursed faster. This aids in keeping their cash flow in check and ensures they have the funds they must keep giving people high-quality care.
Outsourcing to reliable BPO Vendors.
Outsourcing to BPO vendors can help your healthcare practice run smoother. It means handing off tasks like paperwork and billing to experts outside your office. This leaves you more time to focus on your patients and growing your business.
When you work with experienced partners, you can trust that tasks like getting pre-approval for treatments and making sure billing codes are correct will be done accurately and on time. This is important for following industry rules, like HIPAA, and keeping patient information safe.
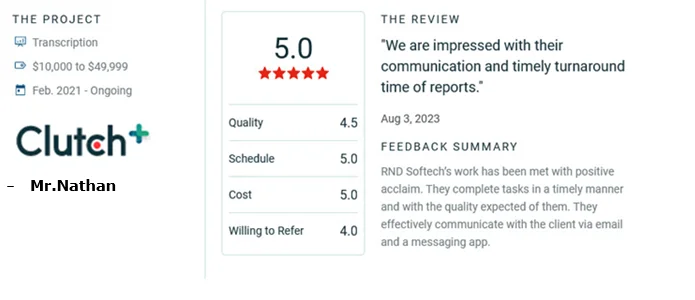
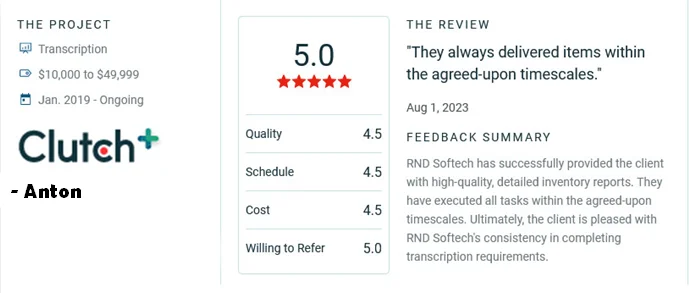
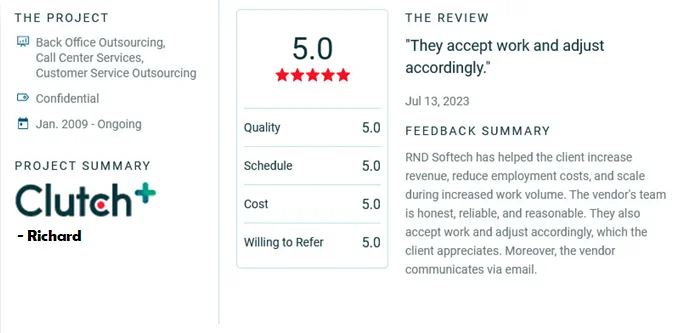
Companies like RND Softech, which has a service track record of 25 years, specialize in helping healthcare practices like yours manage their revenue effectively. They employ data analysis and the newest technology to make sure everything runs smoothly. They can also provide helpful advice based on their experience in the healthcare field.
By outsourcing tasks like billing and paperwork, you can improve your practice's efficiency and ensure you're getting paid for the services you provide.
In conclusion, choosing trusted BPO vendors like RND Softech can transform how you manage your revenue cycle. With skilled experts and advanced technology on your side, you can make your processes more efficient, increase your earnings, and ensure steady progress for your practice. Allow us to assist you in excelling in healthcare administration while you concentrate on providing excellent patient care.
Also, Read our blog - 5 Things To Consider While Outsourcing RCM